Cognitive behavioral therapy (CBT) is a short-term form of psychotherapy that adopts a practical approach to problem-solving. CBT works by changing people’s attitudes and their behavior by focusing on the thoughts, images, beliefs, and attitudes that they hold and how these cognitive processes relate to the way a person behaves, as a way of dealing with emotional problems (Martin, 2018).
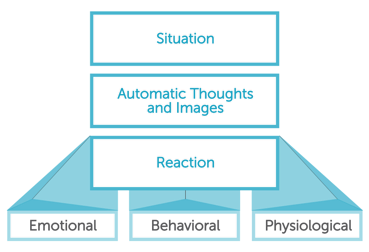
It is based on the cognitive model: the way that individuals perceive a situation is deeply connected to their reaction to it, whether emotional, behavioral or physiological. CBT aims to help you deal with overwhelming problems by breaking them down into smaller parts and allowing you to understand where these problems come from.
CBT is the result of an alliance between the school of behaviorism and cognitive therapy, and was invented by a psychiatrist, Aaron Beck, in the 1960s. As he was doing psychoanalysis, Beck realized that the link between thoughts and feelings was very important, and he concluded that identifying these thoughts was the key to the client understanding and overcoming his or her difficulties (J. Beck, 2011).
CBT favors an equal relationship that is problem-focused and practical, with give and take between the therapist and the client. The therapist will frequently ask the client for feedback and for their views about what is going on in therapy. Finally, the client is also often encouraged to do “homework” such as keeping a diary, or completing small tasks every now and then. Generally, sessions take place once a week or once every 2 weeks. The course of treatment usually lasts for between 5 and 20 sessions, with each session lasting 30 to 60 minutes (NHS, 2016).
Why CBT?
Personally, I think it is a very useful approach in tackling mood problems because it raises the client’s awareness on how their thoughts affect their moods and how the way they think about themselves, others, and the world can lead them into a serious condition, such as depression. It is a practical approach, which focuses on current problems and on the present, whilst acknowledging that it may have been from past experiences that the maladaptive patterns were learned. It looks at what is happening now, and gives tools to manage these moods daily. I am a firm believer in the impact of our own perception and construction of a given situation. These personal perceptions and constructions are what lead to our automatic thoughts, which are the ones we do not reach through reasoning and careful thinking. The danger of these thoughts is that we often do not question them, they just fall on us and we believe them. These automatic thoughts are what will lead to a certain reaction, which is usually the point where the problem is visible with clients who require CBT.
However, automatic thoughts don’t actually fall out of nowhere, and are not that unexpected if we actually look back and try to understand their deeply rooted origins. Often in childhood or early years is when we will acquire our core beliefs, the fundamental beliefs that we have about ourselves or the world and that we no longer question. Examples of those may be “I am not good at…”, “I am not loved”, “I will never get married”, etc. How many times do we hear similar statements in our daily lives?
It is scary to what extent people have self-deprecating beliefs about themselves and to what extent those can harm them on the long run, and eventually appear to be true, in what is known as a self-fulfilling prophecy. Furthermore, core beliefs lead to “intermediate beliefs” which include the rules we set for ourselves, our attitudes, and assumptions. Finally, those are the ones that lead us to our not-so automatic-after-all automatic thoughts.
I think it is crucial for people to realize and gain awareness that 1) they have unhealthy automatic thoughts, 2) these have repercussions on their behavior and emotions and 3) changing the way they think might help solve many of their problems.
CBT is known to be effective in treating many mental health conditions such as anxiety, depression, eating disorders, phobias, OCD and PTSD. There are also very common cognitive distortions present in many clients that seek therapy, such as filtering the good and only seeing the bad, overgeneralizing, thinking in terms of “black or white”, jumping to conclusions, personalization (believing that everything is about them), and catastrophizing. CBT will help them become aware of the flawed reasoning behind these distortions, and put them back on the right track.
Cognitive behavioral therapists, with a new client, begin by creating a cognitive conceptualization for their patient’s case. They ask themselves questions such as:
“How did my patient develop this disorder?”, “What are my patient’s most fundamental beliefs about him/her self and the world?”, “Which automatic thoughts are fueling the disorder?” (J. Beck, 2011).
Part of a session could go a little bit like the following:
- Client: I feel very stressed and nervous in social situations…
- Therapist: Can you tell me more about how you feel around people?
- Client: I feel awkward, shy… I’m afraid of saying the wrong thing, or that people will laugh at me.
- Therapist: Can we try and think of a particular situation connecting your thoughts and your emotions?
- Client: I was very quiet at a work meeting the other day. My boss kept praising my colleagues for their suggestions. I had good suggestions too but was too afraid to share them.
- Therapist: and how did that feel?
- Client: I was sad and frustrated at myself.
- Therapist: and what was going through your mind?
- Client: I guess I felt like I was not good enough, that I would not get any praise, but embarrassment instead.
- Therapist: Okay, so you just exhibited an automatic thought, a thought that just pops into your head and that you feel is true. We feel sad and frustrated, like you said, but we don’t notice the thought behind our emotions. We usually don’t question these thoughts, but I would like to try doing that today, together.
- Therapist: Tell me, when you say: “I am not good enough”, what does that do to your life?
- Client: It makes me angry and frustrated.
- Therapist: So, if you changed your way of thinking, what would that do to your life?
- Client: If I didn’t think I wasn’t good enough anymore? Well, I would be more confident, and happier, I guess.
Conclusion
Finally, CBT comes with some limitations, of course. Firstly, CBT requires commitment. A therapist can help and advise their client, but cannot make their problems go away without their dedication and cooperation. Also, attending regular CBT sessions and doing homework between sessions can be time consuming. Furthermore,
CBT focuses on current problems and current perceptions of things, it doesn’t dig into the past the way psychoanalysis does, and does not address possible unconscious underlying causes of the mental health condition such as childhood trauma or abuse, which I think sometimes may be crucial. CBT, in a way, discards important variables such as family and childhood, and the effect that those can have on a person, even years before the onset of the mental health condition.
Finally, it is a very structured form of therapy, and thus can be overwhelming for some and might feel like a very challenging road to treatment, especially that it requires active work on behalf of the client, not just talking freely about everything that comes to their mind.
References
Beck, J. S. (2011). Cognitive behavior therapy: Basics and beyond (2nd ed.). New York, NY, US: Guilford Press.
Martin, B. (2018). In-Depth: Cognitive Behavioral Therapy. Psych Central. Retrieved from
https://psychcentral.com/lib/in-depth-cognitive-behavioral-therapy/
NHS. (n.d.). Cognitive behavioural therapy (CBT). Retrieved from https://www.nhs.uk/conditions/cognitive-behavioural-therapy-cbt/how-it-works/
The CBT Clinic. (n.d.). Pros and Cons of CBT Therapy. Retrieved from http://www.thecbtclinic.com/pros-cons-of-cbt-therapy